

With the experience gained over the last 3 years of providing extra care to people with co-occurring, as well as experiencing the devastating effects of some not receiving the appropriate level of treatment for all of their conditions, we have decided to create a new programme to address this.
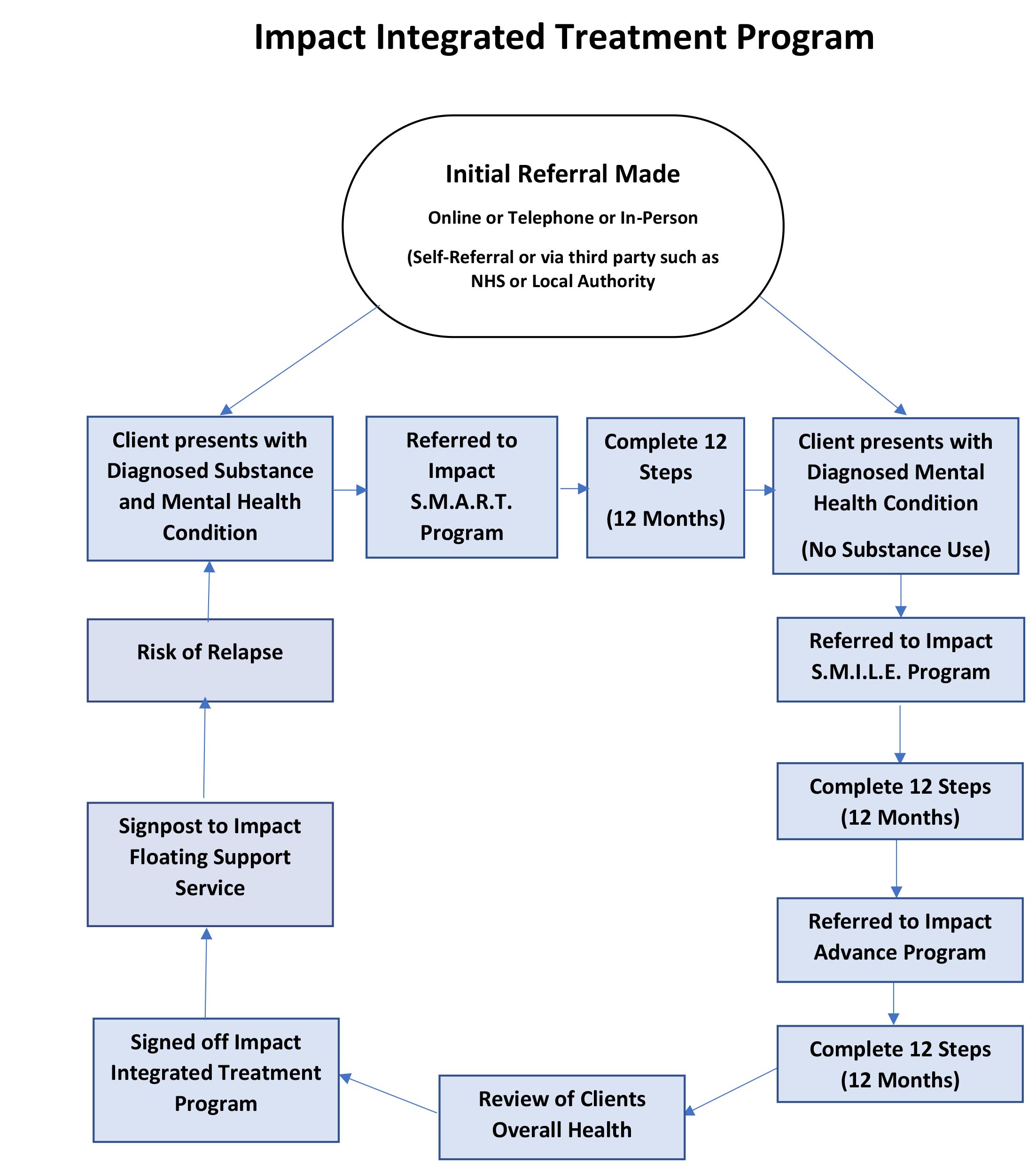
The “Impact Integrated Treatment Program” will include a series of 12-step programs.
The programs will be based on the principles of the ‘integrated treatment model’ for those with dual diagnosis, treating the whole person in the same setting with an interdisciplinary team;
“Integrated treatment takes place when a substance abuse problem is treated at the same time as a mental illness. It approaches treatment with both conditions in mind, knowing that one is often linked to the other.
Studies have shown that 56% of people who deal with mental illness, have a co-occurring substance abuse within their lifetime. Those studies have also shown that by using integrated treatment there are more positive outcomes in the following areas:
– Reduced substance abuse
– Improvement in psychiatric symptoms and functioning
– Decreased hospitalisation
– Increased housing stability
– Fewer arrests
– And overall improvement on the quality of life”
Foundations Recovery Network www.foundationsrecoverynetwork.com/about-us/integrated-treatment-model/
For the Impact Integrated Treatment Program to be effective, it must include the following:
1. Coordinated treatment for multiple disorders
2. A collective of interventions
3. No division between mental health and substance abuse treatments
4. All health professionals collaborating together to prevent contradictory treatments or prescriptions
Success Rates of Integrated Treatment
The integrated model is relatively new, but it has been proven as an effective method in many scientific studies. For example, a study in the Journal of Substance Abuse Treatment found that people who participated in the integrated model had a lower incidence of psychotic episodes and arrests compared to people who did not participate. Their therapy seems to have allowed them to achieve a level of stability, and this resulted in fewer crises.
The integrated treatment model has also been effective in addiction treatment. A study in the journal Hospital and Community Psychiatry found that of 17 people who received inpatient dual diagnosis care, 12 reported continued drug and alcohol abstinence one month later.
It’s clear that integrated treatment models have the capacity to help people gain control over their addictions, their mental illnesses and the other important aspects of their lives. The lessons they learn in therapy can stay with them for the rest of their lives, as they continue to manage both of these chronic conditions over the long term. Relapse is sometimes an issue for these people, as these conditions are powerful and long-term change is hard to sustain; however, therapy provides a strong foundation that can be readdressed as issues occur.
Impact will adapt this model, creating a set of staged programs over a 2-3-year period, which will include steps for the individual to complete each month.
Once the first set of steps and first program has been complete, individuals will then be able to progress to their next set of steps and the second programme and so on until ready for reduced intervention. The staged programs include:
1. Impact SMART Program
o Steps 1-12
2. Impact SMILE Program
o Steps 1-12
3. Impact Advance Program
o Steps 1-12
1. Impact SMART Program
o Steps 1-12
2. Impact SMILE Program
o Steps 1-12
3. Impact Advance Program
o Steps 1-12
Transtheoretical Model
Adapting the ‘Transtheoretical Model’ of treatment founded by Prochaska and DiClemente 1970, Impact’s series of programs will work together to address both the mental health condition and substance use disorder, including steps the individual must complete before progressing to the next program.
The individual’s readiness to act on or make healthier decisions, intentionally, will be continuously assessed as “The TTM operates on the assumption that people do not change behaviours quickly and decisively. Rather, change in behaviour, especially habitual behaviour, occurs continuously through a cyclical process
The TTM posits that individuals move through six stages of change. For each stage of change, different intervention strategies are most effective at moving the person to the next stage of change and subsequently through the model to maintenance, the ideal stage of behaviour.” Boston University School of Public Health. (Please refer to ‘Statistics and Further Research’ for more information on the TTM six stages of change)
Jacey A. Greece, DSc, MPH, sphweb.bumc.bu.edu/otlt/MPH-Modules/SB/BehavioralChangeTheories/BehavioralChangeTheories6.html#headingtaglink_1
Dual Diagnosis and Co-Occurring Disorders
People with both a substance use disorder and a mental health condition are sometimes described as having a dual diagnosis or a co-occurring disorder. These are terms medical professionals use to describe people who have two medical issues impacting them at the very same time.
In the past, GP’s have struggled to determine the right care and type of treatment provider for such people, with debates about how to approach both conditions at once. Often, individuals with a co-occurring disorder have been turned away from support or have only received care for just one of the conditions while other underlying conditions were allowed to grow stronger. Sometimes, individuals have received care from two separate providers where there is a lack of communication or information sharing to enable treatment to work effectively, resulting in being prescribed counter-productive prescriptions, relapse, deteriorating health, suicide or substance related death.
Sadly Impact have become increasingly familiar with co-occurring related deaths within the last year.
We believe that individuals who are not being monitored and managed effectively is part of this reason, as well as the connection between poor mental health leading to substance use disorder and vice versa.
It is often difficult to determine if a person’s thought, behaviour or decision making and subsequent behaviours are related to their mental health condition or substance use disorder, as both conditions may have similar symptoms. It can also be difficult to determine the circumstances or root cause of a mental health condition, particularly if this is due to any other underlying health issues.
Preventing Substance and Mental Illness Co-Occurring Deaths
“Research shows that mental health problems are experienced by the majority of drug (70%) and alcohol (86%) users in community substance misuse treatment. Death by suicide is also common, with a history of alcohol or drug use being recorded in 54% of all suicides in people experiencing mental health problems.
Other evidence tells us that people with co-occurring conditions have a heightened risk of other health problems and early death. We also know that in spite of the shared responsibility that NHS and local authority commissioners have to provide treatment, care and support, people with co-occurring conditions are often excluded from services”
Better Care for People with Co-occurring Mental Health and Alcohol/Drug Use Conditions, Public Health England, June 2017
